Post caesarean section keloids: effectiveness of surgical excision and intralesional triamcinolone acetonide injections for prevention of subsequent recurrence.
Seng Chai Chua, James Brown, Beata Gidaszewski, Marjan Khajehei, Marjan Khajehei
ABSTRACT
Background: Intralesional triamcinolone acetonide (ITA) injection has been used for the treatment of keloids for many decades, but its efficacy in the treatment of caesarean section keloids has not been assessed. This pilot study investigated the efficacy of surgical excision and ITA in the treatment of keloids after caesarean section.
Methods: In this pilot study, 28 patients met the criteria for having a keloid at the site of their previous caesarean section. The keloid lesion was excised at the time of a subsequent caesarean section in the operating theatre. Following excision, 1 mL of triamcinolone acetonide (40 mg/mL) was injected into the upper and lower edges of the wound before its closure. After the intervention, follow-up data were recorded in the patients’ notes and medical notes, which were used for this retrospective study. We used the Kyoto scar scale questionnaire to assess the outcomes based on the information available from all patients from 2006 to 2014.
Funding: None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript. This study was conducted by in-kind support from the Department of Women’s and Newborn Health at Westmead hospital.
Declaration of interests: We declare no conflict of interest.
Introduction
Keloid formation is a common but overlooked issue following caesarean section. A keloid is a benign fibrous lesion that results from an abnormal response to wound healing. 1 In a keloid, the scar tissue grows excessively and invades the skin beyond the original wound. The condition is common, with some authors reporting its presence in 15% of the population. Keloid is particularly prevalent in pregnant and parous women, because pregnancy is the highest independent risk factor for the recurrence of keloid lesions. Women who develop a keloid after their first caesarean section are at increased risk of recurrence with subsequent caesarean section deliveries.
Clinically, keloids result in significant cosmetic disfigurement and discomfort, with patients frequently reporting pruritus, pain, and dysaesthesia. More importantly, caesarean section keloids have a remarkably deleterious effect on quality of life. When lesions are located in areas not usually covered by clothing, 8 they compound the negative impact of caesarean section and are therefore likely to cause further deterioration in a woman’s psychological wellbeing in the post-partum period when mother–child bonding is most important.
Different treatment options have been suggested for keloids with variable success rates, including intralesional corticotherapy, surgical excision, cryosurgery, various forms of irradiation, and combinations of these treatment modalities. Yet, limited research has been undertaken into how to effectively treat keloids following caesarean section. For example, Kim et al. investigated the use of post-operative radiotherapy in a small group of patients and found the treatment to be safe with good cosmetic results, in line with treatment for keloid lesions in general. However, radiotherapy is limited by the need for three fractions, requiring the patient to attend hospital multiple times.
Among the proposed treatments for keloid lesions, intralesional triamcinolone acetonide (ITA) (a corticosteroid) injection, either isolated or in association with other treatments, is suggested for treating keloid lesions. However, its efficacy, in treating caesarean section keloids, has not been assessed. Therefore, we conducted this retrospective study to explore the effect of surgical excision followed by ITA injections on caesarean section keloids.
METHODS
Design and setting
The study was a retrospective cohort study conducted at Westmead hospital in Sydney, New South Wales, Australia.
Ethics
Ethics approval for the retrospective review of data was obtained from Western Sydney Local Health District Human Research Ethics Committee (Ref No. 2019/ETH12877).
INSTITUTIONS
Department of Obstetrics and Gynaecology, Westmead Hospital, Westmead, New South Wales, Australia,
Western Sydney University, Sydney, New South Wales, Australia,
Sydney Medical School, The University of Sydney, Sydney, New South Wales, Australia,
Department of Women’s and Newborn Health, Westmead Hospital, Westmead, New South Wales, Australia,
Department of Women’s and Newborn Health, Westmead Hospital, Sydney, New South Wales, Australia,
Clinical Associate Lecturer, The University of Sydney, Sydney, New South Wales, Australia,
University of New South Wales, Sydney, New South Wales, Australia,
Westmead Medical School, The University of Sydney, Sydney, New South Wales, Australia,
Westmead Hospital, Hawkesbury Rd, Westmead, NSW 2145, Australia,
KEYWORDS
Caesarean section, Keloid lesion, Satisfaction, Surgical excision, Treatment, Triamcinolone acetonide
We identified our study cohort from the electronic maternity database (ObstetriX) used to record perinatal information for all births attended by the first author at the hospital. We identified data for all women who developed a keloid lesion following a caesarean section and subsequently gave birth through a caesarean section at our hospital from October 2006 to January 2014. A total of 29 women with keloids received ITA injections during the study period. The demographic data, obstetric history, characteristics of the keloid lesion after previous caesarean section, details of the caesarean section at the subsequent pregnancy, keloid removal, ITA injection procedure, and follow-up data, were collected as the routine practice and were extracted from ObstetriX. The report was collectively run as an archetype report and saved as a Microsoft Excel datasheet. The one-year follow-up was done as the routine part of the practice and the follow-up data existed in the patients’ medical records before this study’s commencement.
Outcome measure
Keloid lesions at baseline were assessed using the Kyoto scar scale, which is a standardised questionnaire developed by Yamawaki et al. The scale consists of an evaluation of objective signs, including redness, hardness, and elevation (0–1 point each), and subjective symptoms, including pruritus, pain and swelling (0–2 points each). Using the total scores (0–8 points) the results are divided into four grades: excellent (0 points), good (1–2 points), fair (3 points), and poor (4–9 points). According to the patients’ history and criteria for keloid detection, all lesions met the criteria for a keloid. To ensure no inclusion of hypertrophic lesions in our patients, we applied two more criteria: (a) outgrowing after the healing period and not fading with time: outgrowing after the healing period (at least three years after their previous caesarean section) and not fading with time; (b) recurring after surgical excision: the keloids in our multiparous patients (as shown in Figures 1, 2, and 3) recurred after surgical excision at the time of caesarean section.
Procedure
Any red, hard, itching, elevated lesion developing at the site of a previous caesarean section was diagnosed as a keloid. Keloids were excised at the subsequent caesarean section in the operating theatre. Following excision, 1 mL of triamcinolone acetonide (40 mg/mL) (Kenacort-A®; Bristol-Myers Squibb, Inc., NYC) was injected into the upper and 1 mL was injected into the lower edges of the wound, with a 1 mL insulin syringe and a long 25G needle. Subcuticular closure of the wound was performed using subcuticular sutures with 3-0 monocryl for the skin in both the initial and subsequent surgery. No fat tissue was removed.
OPSITE® post-operative dressing (Smith & Nephew, Fort Worth, TX) was applied over the scar. All dressings were removed on day four after the operation. To avoid wound infection, the patients received two doses of intravenous, broad-spectrum antibiotics during the first 24 hours after the operation. All other aspects of the caesarean section surgery and post-operative management of wound care were carried out as per the hospital’s standard protocol. Patients were monitored for any potential side effects and complications during the first six days, with a formal visit six weeks after the operation. Standard caesarean section technique was used, with the same surgeon for the original and subsequent surgeries.
Follow-up
After the intervention, as part of our hospital’s routine obstetrical care and practice, the patients were contacted by phone and invited to a face-to-face visit with the surgeon for the one-year assessment of their keloids. The follow-up data were recorded in the patients’ nursing notes and medical notes and extracted from existing records for this study. Based on the information available in the medical records of all patients from 2006 to 2014, we completed the Kyoto scar scale questionnaire for each patient to assess the outcomes.
Statistical analysis
Data preparation and data cleaning were done in Excel and validated through visual review, value range checks, field type checks, and logical checks by researchers. We performed statistical analyses using SPSS Advanced Statistics, version 24.0 (SPSS, Chicago, IL), and used descriptive statistics to summarise the demographic data. Categorical outcomes before and after the intervention were compared using a χ2 test (or Fisher exact test, where applicable). A one-sample t-test was used to assess continuous non-skewed variables, presented as means with standard deviations. We considered p < 0.05 statistically significant.
Results
Before the intervention, the lesions existed for at least three years after patients’ previous caesarean section. A total of 28 consecutive patients with keloid lesions received surgical excision and ITA injections following their caesarean sections and were followed up at one year after the treatment. Table 1 shows patient demographic data.
Of the 28 participants, three had previously used other remedies such as Bio Oil, Silicone gel, and moisturiser on their lesions before the ITA injection, with no success. After the lesions’ removal and ITA injection, none of the patients used any of these treatments.
Before the ITA injection, 89% of patients had poor grades and 11% had fair grades on the Kyoto scar scale, assessed by symptoms and signs. After the ITA treatment, 36% had excellent outcomes and 21% had good outcomes with significant remission in their keloid (p < 0.001). Forty-three percent had poor-to-fair response to treatment after the first ITA injection (Table 2). There was a significant decline in redness, hardness, elevation, pruritus, pain and swelling after the treatment. The mean score on the Kyoto scar scale was 5 ± 1.5 before treatment versus 1 ± 1.5 one year after. In addition, the mean score on the objective signs and subjective symptoms of the keloid lesions was different before and after the intervention (p < 0.001) (Table 2). Figures 1–4 show pre-treatment keloids and post-treatment results in three patients one year after the operation.
No side effects were reported. Most patients (86%) had a high level of treatment satisfaction: 86% reported that the treatment was worthwhile and 93% stated they would recommend the treatment to others.
Of the 28 women who had keloid treatment at a subsequent pregnancy, four had another ITA injection at their next caesarean section birth. After the second round of treatment, the means and standard deviation scores on the Kyoto scar scale were 0.5 ± 0.6; for objective signs were 0.2 ± 0.4; and for subjective symptoms were 0.4 ± 0.5 (p < 0.05).
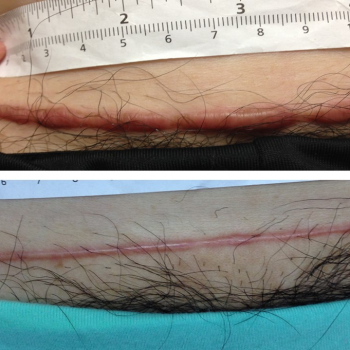
Figure 1: Pre- and post-treatment photographs of caesarean section keloid one year after the operation
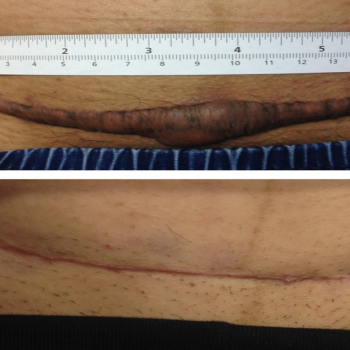
Figure 3: Pre- and post-treatment photographs of caesarean section keloid one year after the operation.
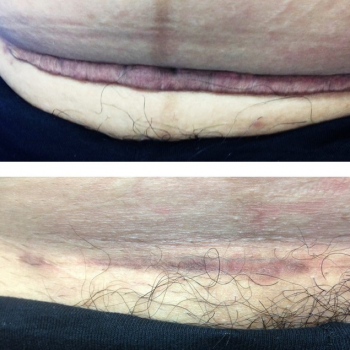
Figure 2: Pre- and post-treatment photographs of caesarean section keloid one year after the operation.
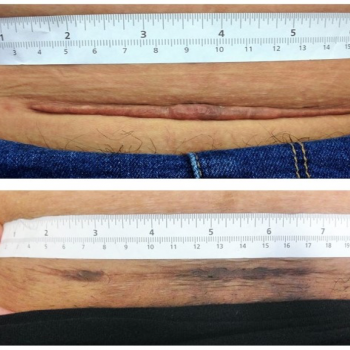
Figure 4: Pre- and post-treatment photographs of caesarean section keloid one year after the operation.
| Baseline data | Frequency (%) (n=28) |
| Age groups (years) 20–29 30–40 | 8 (29%) 20 (71%) |
| Number of previous caesarean sections 1 2 3 | 1 (4%) 25 (89%) 2 (7%) |
| Family history of keloid lesion Yes* No | 5 (18%) 23 (82%) |
| Ethnicity Caucasian North-Eastern Asian South-Eastern Asian Southern Asian | 4 (14%) 13 (47%) 7 (25%) 4 (14%) |
Table 1: Demographic and clinical characteristics of participants
* Mother or maternal uncle
| Characteristic | Before intervention (n=28) | 1 year after intervention (n=28) | p |
| Kyoto scar scale, n (%) Excellent Good Fair Poor | – – 3 (11%) 25 (89%) | 10 (36%) 6 (21%) 8 (29%) 4 (14%) |
< 0.001 |
| Kyoto scar scale, mean (SD) | 5.2 (1.5) | 1.7 (1.5) | < 0.001 |
| Objective signs,* mean (SD) | 2.8 (0.4) | 1.2 (1.3) | < 0.001 |
| Subjective symptoms,¶ mean (SD) | 2.4 (1.4) | 0.4 (0.6) | < 0.001 |
Table 2: Characteristics of keloid lesions before and after treatment
* Including redness, hardness and elevation.
* Including pruritus, pain and swelling.
DISCUSSION
Our study showed that surgical excision followed by ITA appears to be an effective and satisfactory treatment for post-caesarean section keloids with a significant reduction in redness, hardness, elevation, pruritus, pain, and swelling after receiving the treatment. Our results are consistent with previous literature indicating that ITA injection leads to improvement in symptoms in 72% of women and complete lesion flattening in 64% of
cases. Similarly, other research has shown a keloid recurrence rate of < 50% after excision of the lesion and ITA injection. Our study result was higher, perhaps because the retrospective nature of our study contributed to biased outcomes; a large RCT might have different results. Or, our study only investigated the changes in caesarean section keloids. The Pfannenstiel incision causes less wound tension compared to other types of incision, and wound tension has been known to exacerbate keloid formation.
Intralesional corticotherapy suppresses the synthesis of type I collagen and fibronectin by keloid fibroblasts, increases collagenase production and reduces levels of collagenase inhibitors. Reported side effects of systemic corticosteroid injections include severe pain during injection, hypopigmentation, atrophy of skin and subcutaneous fat, and systemic side effects, such as adrenal suppression, steroid acne, and telangiectasia. No side effects were reported by our patients, which supports the hypothesis that ITA treatment can be a low-risk intervention to treat caesarean section keloid lesions. The nil rate of reported side effects could be because ITA generally has a local effect only, and the procedure can be carried out at the time of the subsequent caesarean section.Our study showed high levels of satisfaction with the surgical excision and ITA injections, an important outcome in the context of the impact of keloid lesions on quality of life. Most women (93%) reported that they would recommend the procedure, which indicates their trust in the success of the ITA treatment. These results are in line with studies in other specialties, when ITA was associated with the highest scores for aesthetics and overall satisfaction.
We noted that 43% of patients had poor-to-fair response to treatment after the first surgical excision and ITA injection. This relatively high rate of unsuccessful response to the treatment may be attributed to technical issues, such as ability to evenly distribute the medication through the whole incision lesion. The patient also values the keloid’s symptomatic improvement; the significant decline in redness, hardness, elevation, pruritus, and pain with treatment likely improved patients’ quality of life. This outcome reinforces that the therapeutic effect of keloid lesion treatment extends beyond objectively measurable outcomes.
Limitations, strengths and recommendations for future research
Our study had limitations inherent in the use of administrative data. First, more than one-third of the women had an Asian background. Although this demographic supports previous research that indicates a higher risk of keloid lesions in people with Asian ethnicity, 33 the results may not be generalised to the entire population of women with keloids after caesarean section due to our small sample size. Further large-scale randomised controlled studies are required to investigate the prevalence of keloids in different ethnic groups and to validate the positive effects of ITA on keloids after caesarean section. Second, we assessed the outcomes during the first year after the treatment. Future large randomised studies must follow the women for a longer time to assess the recurrence of symptoms and the women’s long-term satisfaction. Our third limitation is that this was a retrospective pilot study. Due to our promising results, we have used the information from this pilot study to design and commence a randomised controlled trial on the effect of the ITA on subjective and objective improvement of keloids and patient satisfaction. This research protocol has already been published.
Despite these shortcomings, we believe that our study adds to the literature on the treatment of keloids after caesarean section and paves the way for future, high-quality research in a remarkably under-examined area, despite its impact on women’s quality of life.
CONCLUSION
Our study is one of very few to examine the effectiveness and patient satisfaction of treatments specifically for caesarean keloids. The few studies to date reveals a significant lack of knowledge for a common and debilitating condition. We showed that surgical excision followed by ITA injection is an effective treatment for keloids following caesarean section and results in high levels of patient satisfaction.
Acknowledgements
The authors thank Andrew Cheong (Griffith University) and Ben Howes (University of Sydney) for their support of our study.
References
1. Chike-Obi CJ, Cole PD and Brissett AE. Keloids: pathogenesis, clinical features, and management. Seminars in Plastic Surgery. 2009; 23: 178-84.
2. Cohen G, Paghdal KV and Shockman S. Medical and surgical management of keloids: a review. Journal of Drugs in Dermatology. 2010; 9: 1249+.
3. Park T and Chang C. Keloid recurrence in pregnancy. Aesth Plast Surg. 2012; 36: 1271-2.
4. Kim J and Lee SH. Therapeutic results and safety of postoperative radiotherapy for keloid after repeated Cesarean section in immediate postpartum period. Radiation Oncology Journal. 2012; 30: 49-52.
5. Brown BC, McKenna SP, Siddhi K, McGrouther DA and Bayat A. The hidden cost of skin scars: quality of life after skin scarring. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2008; 61: 1049-58.
6. Bock O, Schmid-Ott G, Malewski P and Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Archives of dermatological research. 2006; 297: 433-8.
7. Seifert O and Mrowietz U. Keloid scarring: bench and bedside. Archives of dermatological research. 2009; 301: 259-72.
8. Furtado F, Hochman B, Ferrara SF, et al. What factors affect the quality of life of patients with keloids? Revista da Associacao Medica Brasileira (1992). 2009; 55: 700-4.
9. Torkan B, Parsay S, Lamyian M, Kazemnejad A and Montazeri A. Postnatal quality of life in women after normal vaginal delivery and caesarean section. BMC pregnancy and childbirth. 2009; 9: 4.
10. Mousavi SA, Mortazavi F, Chaman R and Khosravi A. Quality of life after cesarean and vaginal delivery. Oman Medical Journal. 2013; 28: 245-51.
11. Majzoobi MM, Majzoobi MR, Nazari-pouya F, Biglari M and poorolajal J. Comparing quality of life in women after vaginal delivery and cesarean section. Journal of Midwifery and Reproductive Health. 2014; 2: 207-14.
12. Hochman B, Locali RF, Matsuoka PK and Ferreira LM. Intralesional Triamcinolone acetonide for keloid treatment: a systematic review. Aesth Plast Surg. 2008; 32: 705-9.
13. Rousseau JA, Girard K, Turcot-Lemay L and Thomas N. A randomized study comparing skin closure in cesarean sections: staples vs subcuticular sutures. American journal of obstetrics and gynecology. 2009; 200: 265.e1-4.
14. Sharma C, Verma A, Soni A, Thusoo M, Mahajan VK and Verma S. A randomized controlled trial comparing cosmetic outcome after skin closure with 'staples' or 'subcuticular sutures' in emergency cesarean section. Archives of gynecology and obstetrics. 2014; 290: 655-9.
15. Altman AD, Allen VM, McNeil SA and Dempster J. Pfannenstiel incision closure: a review of current skin closure techniques. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2009; 31: 514-20.
16. Cromi A, Ghezzi F, Gottardi A, Cherubino M, Uccella S and Valdatta L. Cosmetic outcomes of various skin closure methods following cesarean delivery: a randomized trial. American journal of obstetrics and gynecology. 2010; 203: 36.e1-8.
17. Mackeen AD, Devaraj T and Baxter JK. Cesarean skin closure preferences: a survey of obstetricians. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2013; 26: 753-6.
18. Kim J and Lee SH. Therapeutic results and safety of postoperative radiotherapy for keloid after repeated Cesarean section in immediate postpartum period. Radiation oncology journal. 2012; 30: 49-52.
19. van Leeuwen MCE, Stokmans SC, Bulstra AEJ, et al. Surgical excision with adjuvant irradiation for treatment of keloid scars: a systematic review. Plastic and Reconstructive Surgery – Global Open. 2015; 3: e440.
20. Al-Attar A, Mess S, Thomassen JM, Kauffman CL and Davison SP. Keloid pathogenesis and treatment. Plastic and reconstructive surgery. 2006; 117: 286-300.
21. Yamawaki S, Naitoh M, Ishiko T, Muneuchi G and Suzuki S. Keloids can be forced into remission with surgical excision and radiation, followed by adjuvant therapy. Annals of plastic surgery. 2011; 67: 402-6.
22. Yamawaki S, Naitoh M, Yoshikawa K, Ishiko T and Suzuki S. Kyoto scar scale for assessment of keloids following surgery and irradiation. Sosyo. 2011; 2: 112-7.
23. Darzi MA CN, Kaul SK, Khan M. Evaluation of various methods of treating keloids and hypertrophic scars: a 10-year follow-up study. . Br J Plast Surg. 1992;45: 374-9.
24. Kauh YC, Rouda, S., Mondragon, G., et al. Major suppression of pro-alpha1(I) type I collagen gene expression in the dermis after keloid excision and immediate intrawound injection of triamcinolone acetonide. . J Am Acad Dermatol 1997; 37: 586.
25. Kuo YR WW, Jeng SF, et al. Activation of ERK and p38 kinase mediated keloid fibroblast apoptosis after flashlamp pulsed-dye laser treatment. Laser Surg Med. 2005; 36: 31–7.
26. Cruz NI, and Korchin, L. Inhibition of human keloid fibro- blast growth by isotretinoin and triamcinolone acetonide in vitro. Ann Plast Surg. 1994; 33: 401.
27. Boyadjiev C, Popchristova, E., and Mazgalova, J. . Histomorphologic changes in keloids treated with Kenacort. J Trauma. 1995; 38: 299.
28. Niessen FB, Spauwen, P. H., Schalkwijk, J., and Kon, M. On the nature of hypertrophic scars and keloids: A review. Plast Reconstr Surg 1999; 104: 1435.
29. Mustoe TA CR, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, et al. International clinical recommendations on scar management. . Plastic and reconstructive surgery. 2002; 110: 560–71.
30. Friedman SJ, Butler, D. F., and Pittelkow, M. R. Perilesional linear atrophy and hypopigmentation after intralesional corti- costeroid therapy: Report of two cases and review of the literature. J Am Acad Dermatol. 1988; 19: 537.
31. Bijlard E, Kouwenberg C, Timman R, Hovius S, Busschbach J and Mureau M. Emotional quality of life is severely affected by keloid disease: pain and itch are the main determinants of burden. A CLINICAL STUDY. 2017; 97: 25.
32. Hickey S, Brown D, Levin J, et al. 327 Treatment of keloids with CO2 Fractional photothermolysis, intralesional, and topical steroids. Journal of Burn Care & Research. 2018; 39: S133-S.
33. Kim S, Choi T, Liu W, Ogawa R, Suh J and Mustoe T. Update on scar management: guidelines for treating Asian patients. Plastic and reconstructive surgery. 2013; 132: 1580-9.
34. Chua S, Gidaszewski B and Khajehei M. Efficacy of surgical excision and sub-dermal injection of triamcinolone acetonide for treatment of keloid scars after caesarean section: a single blind randomised controlled trial protocol. Trials. 2019; 20: 363.
