Impact of COVID-19 on Keloids - Case Report
[Version 2. Awaiting Peer Review. Approved For Rapid Publication]
Michael H. Tirgan, MD
ABSTRACT
The COVID-19 pandemic impacted the delivery of healthcare services and medical treatments to many patients, including those with benign skin conditions such as keloids. However, direct impact of the COVID-19 illness on the biology of the keloid disorder has not been previously reported in the literature. This case report describes a 23-year-old male patient who, on the fifth day of becoming symptomatic with COVID-19, developed a noticeable swelling at the site of previously treated chestkeloid that resolved spontaneously with resolution of the underlying COVID-19.
To the author’s knowledge, direct impact of COVID-19 disease on the biology ofkeloid disorder has not been previously described.
INTRODUCTION
Pathophysiology of keloid disorder (KD) is complex and in part due to abnormalities in the wound-healing mechanism [1]. Inflammation - an important component of the normal wound-healing response – is a critical component of the pathophysiology of KD. Usage of intra-lesional steroids was first reported by Dr. Schleyer-Saunders in 1968 who hypothesized and harnessed on the anti-inflammatory effects of steroids in the treatment of keloids [2].
The COVID-19 infection triggers a dysregulated, inflammatory immune response with significant cytokine release that can progress to a state of hyperinflammation, ultimately resulting in tissue damage, organ failure, and even death [3]. The key consequence of this cytokine release is progressive, widespread, systemic inflammation [3,4].
Much of the research on the role of inflammation in keloid pathology has been focused on the localized inflammation occurring at the site of visible keloid lesions [5,6].
The COVID-19 pandemic has had a direct impact on the delivery of healthcare services to patients with benign medical conditions, [7] including patients with keloids [8]. As of yet, there has been no reports of COVID-19 directly impacting the pathophysiology of KD. To the author’s knowledge, this is the first report of COVID-19 directly impacting the biology of KD.
CASE REPORT
The male patient described here was born in January 1998. At age 15, papular and nodular keloids started to form on his chest. Over the next several months, despite treatment with intralesional steroids, the chest keloids continued to grow and increase in size and number.
In October 2018, at the age of 20 years, the patient presented to the author with several nodular keloids on his anterior chest region (Figure 1A). The nodular lesions were initially treated with contact cryotherapy. Then, in accordance with the published KRF guidance, intralesional chemotherapy was used once every 2-3 months with three different chemotherapeutic drugs [9]. This resulted in partial improvement of the lesions by May 2019 (Figure 1B). Treatment was maintained throughout 2019, and incremental improvement was achieved. Figure 1C depicts the extent of improvements achieved by March 2020, when patient was last seen prior to the pandemic, and treated with intralesional chemotherapy.
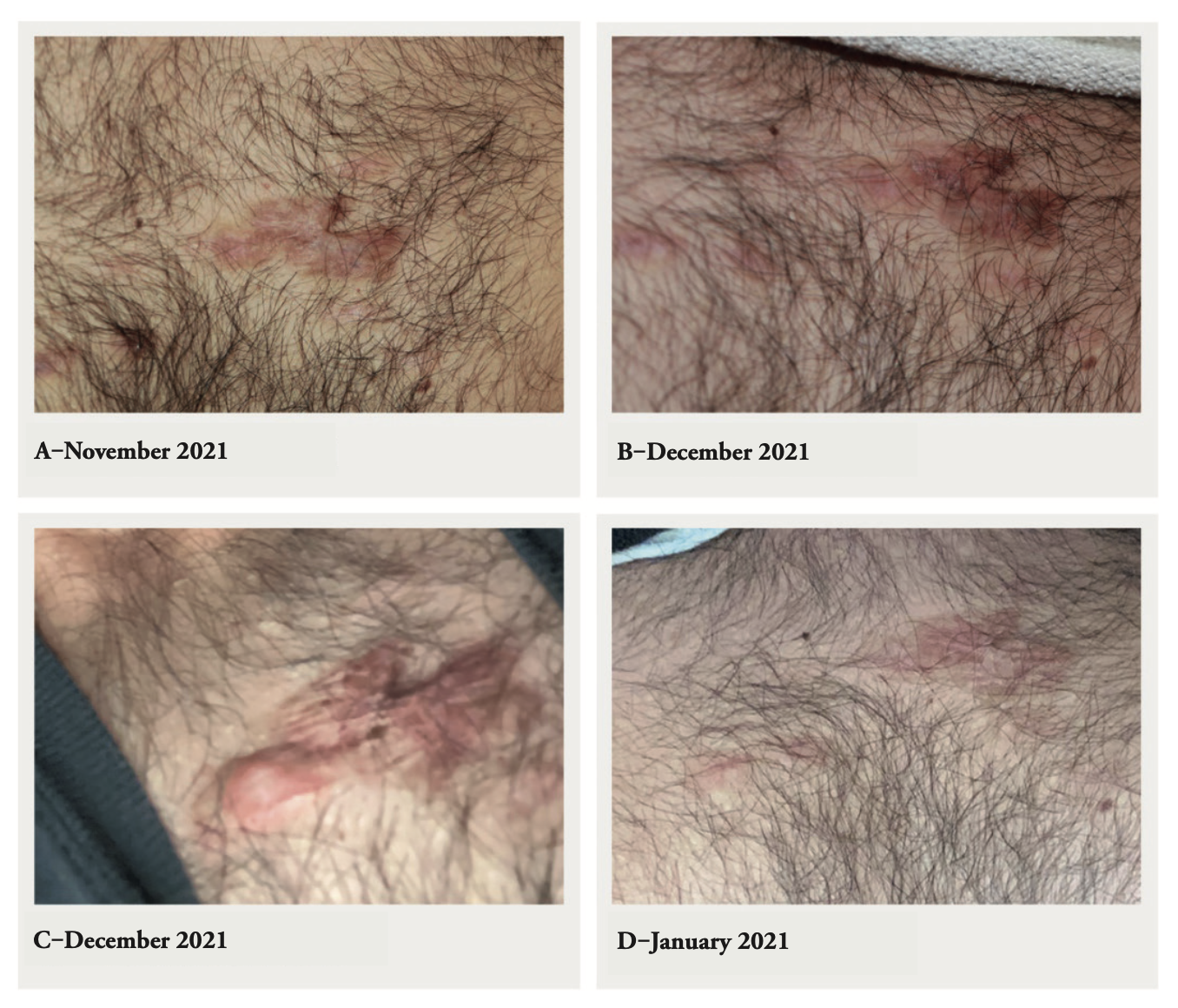
Treatment was interrupted due the COVID-19 pandemic in early 2020. The patient did not return for follow-up until February 2021. Several of his keloid lesions had remained flat, despite not having received any treatment for almost one year (Figure 1D); only two prominent keloid recurrence sites were found. Intralesional chemotherapy treatment was resumed on a regular basis, and almost complete remission was achieved by November 2021 (Figure 2A).
Due to planned, long-term travel, the remaining keloid lesions were treated with intralesional chemotherapy on November 6, November 18, and December 2, 2021. Figure 2B depicts the appearance of the keloids during the last visit on December 2, 2021.
The patient began exhibiting symptoms of COVID-19 on December 3, 2021. His symptoms included chills, severe headaches, rigors, body aches, and rhinorrhea. The patient took a COVID PCR test on December 5, 2021, and the results were positive. While symptomatic with moderate flu-like symptoms, patient noticed a rapid-onset growth at the site of his previously flattened chest keloids. Figure 2C depicts the appearance of the new onset keloid-like growth as well as generalized erythema of the previously treated keloid lesions. This image was taken on December 9, 2021 by the patient using a low resolution cell phone camera.
The location of the growth was at a previously flattened keloid site that had responded well to past treatment. The swelling was described by the patient as non-tender, painless, and solid. To rule out keloid tissue infection, the patient was advised to monitor the site over the next 24-48 hours. Over the next several days, the lesion remained painless and gradually softened, showing signs of regression. By January 17, 2022, complete regression was achieved without any interventions (Figure 2D), and the patient’s COVID-19 symptoms had fully resolved.
FIGURE 1:
1A. Anterior chest keloids at presentation in October 2018.
1B. Chest keloids responding to intralesional chemotherapy, May 2109
1C. Partial response to intralesional chemotherapy, March 2020
1D. Appearance after a treatment gap of close to one year, February 2021.
FIGURE 2:
2A. Near-complete flattening of keloids, November 18, 2021.
2B. Near-complete flattening of keloids, December 2, 2021.
2C. Rapid onset swelling at the site of previously treated and totally flattened chest keloid, December 9, 2021. Image was taken by the patient, while in quarantine for symptomatic COVID-19 infection.
2D. Complete regression of swelling following recovery from COVID-19, January 17, 2022. Image was taken by the patient.
DISCUSSION
Rapid onset swelling of the keloid tissue is most often due to an infectious process, often presenting with new onset pain and tenderness, as well as erythema of the keloid tissue and the adjacent skin. This patient had no signs or symptoms that would indicate an infected keloid. This led the author to believe that the dysregulated, inflammatory immune response associated with significant cytokine release from COVID-19 infection had triggered the sudden onset of swelling in the flattened areas of this patient’s previously treated chest keloids. Such a rapid reaction to COVID-19 infection in a treated or untreated keloid lesion has to the author’s knowledge not been reported previously.
Furthermore, what is perhaps most noteworthy is that the swelling occurred in only one area, while the rest of the previously treated keloid lesions did not react in the same manner. Whether such a localized reaction indicates the presence of residual keloid tissue at this particular site may only be answered by simple follow-up, without further interventions. The patient is being followed clinically without any further keloid-directed treatments. The patient remains in good health as of February 8, 2022, and his chest keloids are flat and asymptomatic.
References
- Blažić TM, Brajac I. Defective induction of senescence during wound healing is a possible mechanism of keloid formation. Medical hypotheses. 2006;66(3):649-652. doi:10.1016/j.mehy.2005.09.033
- Schleyer-Saunders E. Keloids. Br Med J. 1968 Nov 2;4(5626):325. doi: 10.1136/bmj.4.5626.325-b. PMID: 5687974; PMCID: PMC1912303.
- Tomerak S, Khan S, Almasri M, et al. Systemic inflammation in COVID-19 patients may induce various types of venous and arterial thrombosis: A systematic review. Scandinavian journal of immunology. 2021;94(5). doi:10.1111/sji.13097
- Reddy K, Rogers AJ, McAuley DF. Delving beneath the surface of hyperinflammation in COVID- 19. Lancet Rheumatol. 2020;2:e578-e579.
- Limandjaja GC, Niessen FB, Scheper RJ, Gibbs S. The Keloid Disorder: Heterogeneity, Histopathology, Mechanisms and Models. Front Cell Dev Biol. 2020 May 26;8:360. doi: 10.3389/fcell.2020.00360. PMID: 32528951; PMCID: PMC7264387.
- Ogawa, R. (2017). Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int. J. Mol. Sci. 18, 1–10. doi: 10.3390/ijms18030606
- Werner RM, Glied SA. Covid-Induced Changes in Health Care Delivery — Can They Last? The New England journal of medicine. 2021;385(10):868-870. doi:10.1056/NEJMp2110679
- Carter AR, Davies BM, Brindley DA. Gazing Long into a Clinical and Social Abyss? Treating Hypertrophic Scarring and Keloids. Rejuvenation Res. 2021 Aug;24(4):307-309. doi: 10.1089/rej.2021.0037. Epub 2021 Jul 8. PMID: 34155931; PMCID: PMC8403195.
- Tirgan, MH, KRF Clinical Practice Guidelines in Keloid Disorder (KRF Guidelines®) Intra-Lesional Chemotherapy, Version 1.2018, Keloid Research. Dec. 10, 2018. Journal of Keloid research. Special Edition, April 1, 2019 (https:// www.keloidresearch.com/krf-clinical-practice-guidelines- keloid-disorder-krf-guidelines-intra-lesional-chemotherapy- version-1-2018/)
METRICS
Impact of COVID-19 on Keloids - Case Report
Michael H. Tirgan, MD
Keloid Research Foundation
23 West 73rd Street, Suite GD, New
York, NY 10065
(212) 874-4200
Tirgan@KeloidResearchFoundation.org
Conflict of Interest
None
Funding
None
Word Count
1328
IRB appRoVal
N/A. Patient provided a written consent to publish this report.
Keywords
COVID, Keloid, Surgery