Bilateral Posterior Subcapsular Cataract in a Patient with Sternal Keloid Treated with Intralesional Corticosteroids.
Tajinder Pal Singh MD, Tarun Narang MD, MNAMS
ABSTRACT
Background: Development of posterior subcapsular cataracts following systemic corticosteroids is well described but not after intralesional extraocular corticosteroid injection. We report a case of bilateral posterior subcapsular cataract in a patient with a sternal keloid treated with multiple doses of intralesional triamcinolone acetonide injection.
Case: A 35-year-old male patient developed blurring of vision in both eyes one year after treatment with multiple injections of intralesional triamcinolone acetonide for sternal keloid disorder. He was diagnosed with bilateral posterior subcapsular cataracts, with best corrected visual acuity of 6/18 in both eyes.
Conclusion: Posterior subcapsular cataracts are well known to occur after systemic corticosteroids, but they may develop after intralesional corticosteroid treatment as well.
Introduction
Posterior subcapsular cataracts are a well-known complication of oral, intravenous, and topical (ocular) corticosteroids. Cataract formation following extraocular intralesional corticosteroids has not been reported previously, although there are case reports of cataract following topical corticosteroids used for dermatological conditions. We report a case of bilateral posterior subcapsular cataracts in a young, non-diabetic male patient with a large sternal keloid treated with multiple doses of intralesional injections of triamcinolone acetonide.
Case description
A 35-year-old, non-diabetic male patient presented with blurring vision in both eyes, which had developed in the previous six months. A large sternal keloid was seen on examination, which had flattened following treatment. The patient provided a history, which included past treatment with as many as eight intralesional triamcinolone acetonide injections by a dermatologist (Figure 1). The patient had no history of bronchial asthma, any other dermatological disorder or systemic corticosteroid treatment in any other form. The patient also had no history of wearing glasses; his best-corrected visual acuity (BCVA) was 6/18 in both eyes. An anterior segment examination showed the presence of posterior subcapsular cataracts in both eyes, with a quiet anterior chamber (figures 2A and 2B). Intraocular pressure (IOP), using Goldmann applanation tonometry, was 16 mm of Hg in the right eye and 18 mm of Hg in the left eye. A posterior segment examination, using slit-lamp biomicroscopy, showed a healthy optic disc with a cup to disc ratio of 0.3:1 and normal foveal reflex, with clear vitreous in both eyes. No peripheral retinal lesion and pars plana snowball opacities were noted on indirect ophthalmoscopic examination. The patient was advised to undergo cataract surgery with intraocular lens implantation in both eyes.
INSTITUTIONS
Department of Ophthalmology, ESIC Model Hospital, Baddi, Himachal Pradesh, India,
2Department of Dermatology, Venereology and Leprology, PGIMER, Chandigarh, India,
KEYWORDS
Keloids; intralesional corticosteroids; triamcinolone acetonide. Posterior subcapsular cataract

Figure 1: Photograph showing a large sternal keloid lesion.
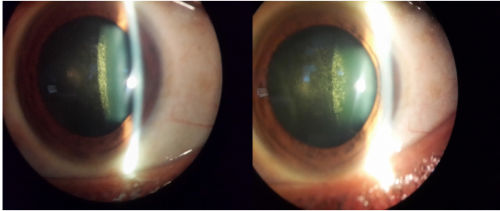
Figures 2A & 2B: Posterior subcapsular cataract in (A) right eye and (B) left eye by slit-lamp biomicroscopy.
DISCUSSION
Intralesional corticosteroids are the most frequently used treatment for keloid disorder and triamcinolone acetonide is the most frequently used agent. The response rate of triamcinolone acetonide injections in keloids has been shown to be as high as 65% Local complications of intralesional steroid injections, such as hypopigmentation, skin atrophy, telangiectasia and ulceration has also been noted in up to 63% of patients. Systemic complications are rare, but Cushing’s syndrome after keloid treatment with intralesional steroids has been reported by various authors
An international panel of experts has recommended triamcinolone acetonide concentrations of 2.5-20 mg/ml for face and 20-40 mg/ml for body keloids. Most patients in case reports for Cushing’s syndrome after intralesional steroids for keloid treatment were given doses larger than 40 mg within a month. Our patient received eight injections of triamcinolone acetonide over a period of six months. It is possible that the cumulative dose may be above the threshold and systemic absorption might have resulted in the formation of typical posterior subcapsular cataract in both eyes.
Hietanen et al., in their retrospective study, found that intralesional triamcinolone acetonide is ineffective in curing large keloids and thus advised limiting the total number of injections to a maximum of four. Therefore, in a large keloid lesion, like that of our male patient, the treating dermatologist / physician should be wary of systemic side effects of steroid injections like cataracts. The accumulative dose of intralesional steroids should be limited and other treatment modalities chosen such as cryoablation or intralesional 5-Fluorouracil.
CONCLUSION
intralesional triamcinolone acetonide injections for keloid disorder may lead to cataract formation, as seen with corticosteroid administration through other routes. Therefore, overenthusiastic treatment in the form of too many injections or increased doses of steroids should be avoided, especially in large keloids lesions.
Financial support and sponsorship
Nill
CONFLICT OF INTEREST
No conflict of interest.
References
1. Tatham A. Atopic dermatitis, cutaneous steroids and cataracts in children: two case reports. J Med Case Rep. 2008; 2:124.
2. Hietanen K, Vaelisuo P, Kuokkanen H, Kaartinen I. Long-term results of intralesional triamcinolone acetonide injections in keloid treatment. J Clin Trials 2016; 6:278.
3. International clinical recommendations on scar management. Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, Stella M, Téot L, Wood FM, Ziegler UE; International Advisory Panel on Scar Management. Plast Reconstr Surg. 2002; 110(2):560-71.
4. Fredman R, Tenenhaus M. Cushing’s syndrome after intralesional triamcinolone acetonide: a systemic review of literature and multinational survey. Burns 2013; 39(4):549-57.
5. Liu MF, Yencha M. Cushing’s syndrome secondary to intralesional steroid injections of multiple keloid scars. Otolaryngol Head Neck Surg 2006; 135(6):960-1.
6. Gold MH, McGuire M, Mustoe TA, Pusic A, Sachdev M, Waibel J, Murcia C; International Advisory Panel on Scar Management. Updated international clinical recommendations on scar management: part 2-algorithms for scar prevention and treatment. Dermatol Surg. 2014; 40(8):825-31
